Fibromyalgia And Depression, What Is The Relationship?
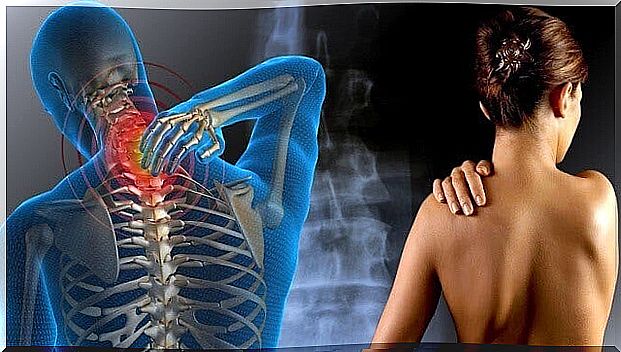
Fibromyalgia is a syndrome characterized by the presence of chronic generalized musculoskeletal pain. In addition to pain, other symptoms are associated, such as fatigue, sleep disturbances, paraesthesia in the extremities, a sensation of swelling in the hands or morning stiffness.
So far there is no therapy / intervention that cures fibromyalgia, so existing treatments focus exclusively on mitigating or cushioning the impact of different symptoms, such as pain, sleep problems or emotional distress.
With regard to psychopathology, it has been observed that the prevalence of depression is higher in the group of patients with fibromyalgia than in the rest of the patients. Thus, in this article we will delve a little deeper into this relationship.
What happens before, fibromyalgia or depression?
There are lines of research that describe a possible relationship between pain and certain personality variables, finding evidence that supports the theory that there is a high relationship between some personality traits and chronic pain.

On the other hand, a high incidence of depressed mood is also observed among patients with pain, frequently assuming that it is the mood that causes it.
Among the pain-related disorders, we are going to focus on fibromyalgia. A rheumatological syndrome characterized by generalized pain, which is considered chronic and whose main symptom is central sensitization that manifests itself as diffuse pain that affects the whole body.
Among the causes of this syndrome, factors of an emotional nature have been proposed, among others. In this sense, the implication of emotional variables, such as anxiety or depression, is recognized, finding that 30% of patients with fibromyalgia present depression when they come to the consultation and 60% suffer it at some point in their medical history . Even so, the impact of these emotional disorders on the etiology or maintenance of fibromyalgia is not clear.
What does the research say about the relationship between fibromyalgia and depression?
In 2004, an investigation was launched at the University of the Balearic Islands whose objective was to corroborate the relationship between fibromyalgia and depression. The authors sought to verify whether patients suffering from fibromyalgia present a specific profile in the manifestation of this mood disorder.
In relation to depression, it was observed that there were no significant differences between patients suffering from fibromyalgia and healthy patients. This could be a sign that depression may precede or accompany fibromyalgia, although it is not a factor involved in the etiology (cause) of the syndrome.
What does seem to be true is that the existence of a relationship between fibromyalgia and depression is more a matter of comorbidity (both disorders appear at the same time), or that the depressed mood may be a consequence of fibromyalgia. In this sense, the depressed mood in patients with fibromyalgia would be a consequence of the interference of pain and other symptoms in daily life.
Symptoms of the syndrome (for example, fatigue) would prevent activities that had been habitual up to now, as well as lead the person to inhibit themselves from participating in certain projects due to the anticipation of pain. This would lead to a loss of reinforcers or motivating stimuli in the patient’s daily life, which would end up triggering the depressive disorder.
What implications does this relationship have for professional practice?
To carry out prevention in depression we can use various tools such as the following:
- Reflect on our way of life. The key is to incorporate rewarding activities and improve your social life. Taking into account that these patients have specific difficulties, activities should be chosen according to their abilities.
- Identify what our way of thinking is like and try to change the thoughts that make us feel bad, replacing them with less harmful ones.
- Use workshops or therapeutic groups. Knowing other people who are going through the same thing as you helps you feel understood and acquire some really useful tools for your problem in question.
- Going to the psychologist is always an option.
Thus, the results obtained may have important implications for professional practice. If depression is not a cause, but a consequence of fibromyalgia, this could lead to the development of specific prevention programs -based on the tools we have described- for this population.